Making Bangladesh a world-class health hub

Every year, over 450,000 Bangladeshi patients travel overseas for medical treatment, spending approximately $5.0 billion per annum. These statistics do not include those who travel on tourist visas for treatment.
Until recently, the most common destinations for Bangladeshi patients seeking medical treatment have been India, followed by Thailand and Singapore, with Western countries being a rarer choice. Over half of India's medical tourists are reported to be from Bangladesh.
A study conducted in 2023 on Bangladesh's medical tourism has revealed several reasons why well-off Bangladeshis prefer treatment abroad rather than locally. These include, but are not limited to:
(i) lack of trust in the Bangladeshi healthcare system;

(ii) inadequate or outdated medical resources, logistical inefficiencies, and long waiting times; and
(iii) perceived cost-effectiveness and better care, including the more compassionate bedside manner of doctors and health workers abroad.
This article further explores the factors driving medical tourism among Bangladeshis and proposes remedial measures that could restore quality within the Bangladeshi healthcare system. In doing so, it aims to redirect the annual $5.0 billion spent on overseas medical treatment back into the country's own healthcare sector.
BUILDING TRUST
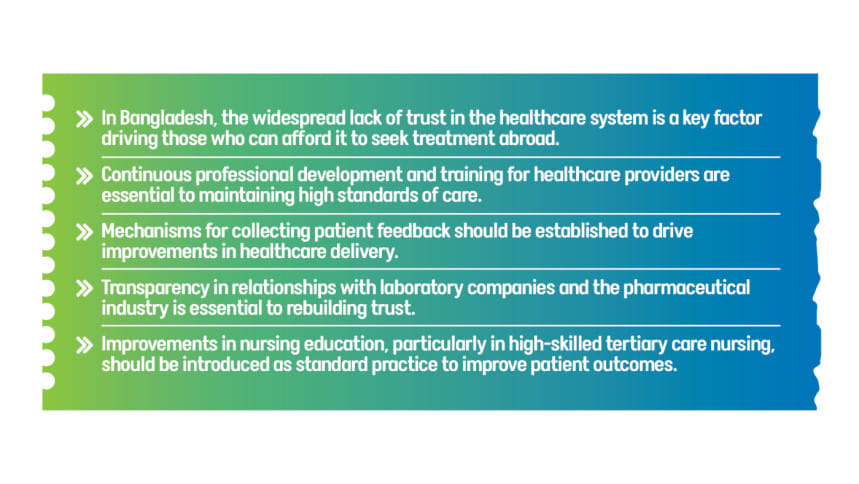
Trust is a fundamental pillar of confidence in a country's healthcare system. It plays a crucial role in ensuring the effective functioning and appeal of medical services. In Bangladesh, a significant lack of trust in the healthcare system is a primary reason why those who can afford it opt for treatment abroad.
Mistrust in Bangladesh's healthcare system stems from several factors, the most significant of which include:
(i) conflicting medical advice;
(ii) inappropriate and/or inadequate use of medical resources; and
(iii) lack of communication skills and/or inappropriate communication methods among healthcare professionals.
Reports of unethical behaviour, including conflicts of financial interest, have further eroded trust in the system and damaged the reputation of healthcare professionals in Bangladesh. One such widely held perception of abuse relates to hospital admission rights and the inappropriate use of medical resources, including intensive care units. For instance, terminally ill patients with no clinical prospects of recovery are often placed on ventilation without due consideration for proper end-of-life care options.
Alleged underhand commercial links between attending doctors, hospitals, testing laboratories, and the pharmaceutical industry—resulting in unnecessary and expensive tests and treatments—place a heavy financial burden on patients and discourage them from seeking medical care locally.
Additionally, widespread allegations of corruption among health administrators and policymakers responsible for quality control have further exacerbated public mistrust in the healthcare system.
In sum, building trust in the healthcare system is an urgent necessity, requiring measures that address a wide range of issues, from improving doctor-patient relationships to incentivising ethical medical practice.
IMPROVING DOCTOR-PATIENT COMMUNICATION
Effective communication is the cornerstone of a successful doctor-patient relationship. In Bangladesh, patients often feel that their concerns are not adequately heard or addressed. This perception is exacerbated by limited consultation times and the overwhelming patient loads that healthcare professionals face daily.
The high patient-to-doctor ratio in Bangladesh means that doctors are often unable to spend sufficient time with each patient. This results in rushed consultations, where patients feel that their issues are neither thoroughly examined nor understood. Consequently, they often feel neglected and perceive that they do not receive value-for-money services.
Such negative experiences further erode trust and confidence in the local medical system. The sheer volume of patients that doctors must attend to daily contributes to the perception of inadequate care. This overwhelming workload can also lead to burnout among healthcare providers, further diminishing the quality of care.
Therefore, while efforts must be made to increase the number of healthcare providers, improving doctor-patient communication is crucial in rebuilding trust. Specialised training should be introduced to equip healthcare professionals with effective communication skills, ensuring that patients feel heard, understood, and cared for.
INSTITUTIONALISING PRIMARY/SPECIALIST CONSULTATION PROCESSES
Furthermore, the absence of a robust primary healthcare system and referral process often results in delayed or missed diagnoses. Patients frequently bypass primary care and seek specialist consultations directly, leading to fragmented and inefficient care.

INCENTIVISING DOCTORS/HEALTHCARE PROVIDERS
Building trust in healthcare services in Bangladesh also requires addressing issues that affect the morale of doctors and healthcare workers. Low morale among doctors stems from inadequate remuneration, job uncertainty, and the public blaming them for systemic failures despite their hard work and dedication.
Over-politicisation, nepotism, and discrimination further hinder physicians' ability to provide quality care. A culture of mistrust has developed, with healthcare professionals frequently facing mob justice for systemic failures. Many doctors feel constrained by substandard conditions in public hospitals and a lack of modern technological support, including proper record-keeping systems.
THE REFORM AGENDA
The intricate interplay between patients, healthcare providers, and policymakers necessitates urgent reforms in the Bangladeshi healthcare system. By addressing systemic issues related to communication, education, regulation, and trust, an improved healthcare environment can be established, ultimately benefiting both patients and healthcare professionals. These changes are crucial for fostering a healthcare system that is effective, reliable, and capable of meeting the needs of the population.
Below are some suggestions for policymakers to consider:
1. Significant gaps remain in Bangladesh's healthcare regulations, including, among other things, inconsistent and often inadequate training of professionals, as well as overall poor standards that continue to plague the quality of healthcare service delivery in the country. The lack of stringent regulatory oversight allows substandard healthcare facilities and practices to persist.
2. Continuous professional development and training for healthcare providers are essential to maintaining high standards of care. Investment in medical education will ensure that healthcare professionals remain up to date with the latest advancements and evidence-based practices. Ongoing training and professional development for doctors should be prioritised to elevate standards of care. This includes training in communication, empathy, and the latest medical advancements.
3. Mechanisms for collecting patient feedback should be established to drive improvements in healthcare delivery. Patient-reported outcomes offer valuable insights into areas that need attention. Prompt and impartial resolution of patient complaints is crucial for building trust in the healthcare system.
4. Clear guidelines and policies should be established to address conflicts of interest. Transparency in relationships with laboratory companies and the pharmaceutical industry is essential to rebuilding trust. Establishing a regulatory body (such as Medicine Australia) could oversee the responsible and ethical engagement of the industry.
5. Healthcare policies should shift towards measuring patient-reported outcomes for continuous improvement. This patient-centred approach will ensure that the healthcare system is responsive to the needs and concerns of patients. Introducing essential specialities such as geriatric medicine, emergency medicine, and perioperative medicine should be a priority. Supporting local medical research is also crucial for healthcare development.
6. Improvements in nursing education, particularly in high-skilled tertiary care nursing, should be introduced as standard practice to improve patient outcomes. Highly skilled integrated allied health services are also essential for overall healthcare achievement.
7. The adequate use of multidisciplinary team (MDT) meetings for improved patient outcomes should be a fundamental component of any modern healthcare system.
8. Establishing a regulatory authority for recognising skill-based sub-specialities in medicine, such as endoscopic or surgical procedures, is necessary for maintaining high standards of care.
Last but not least, incentivising healthcare providers to deliver high-quality services is essential. Self-reflection and a willingness to improve, along with seeking support—particularly from expatriate Bangladeshi doctors worldwide who are eager to contribute—will be instrumental in achieving a trustworthy, patient-friendly, and cost-effective healthcare system in Bangladesh that we can all take pride in.
Note: This article is a revised version of the original piece, The Cost of Mistrust, published in Panacea by the Society of Bangladeshi Doctors, Queensland (SBDQ), Australia.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 


Comments