Management of diabetes-related foot infections
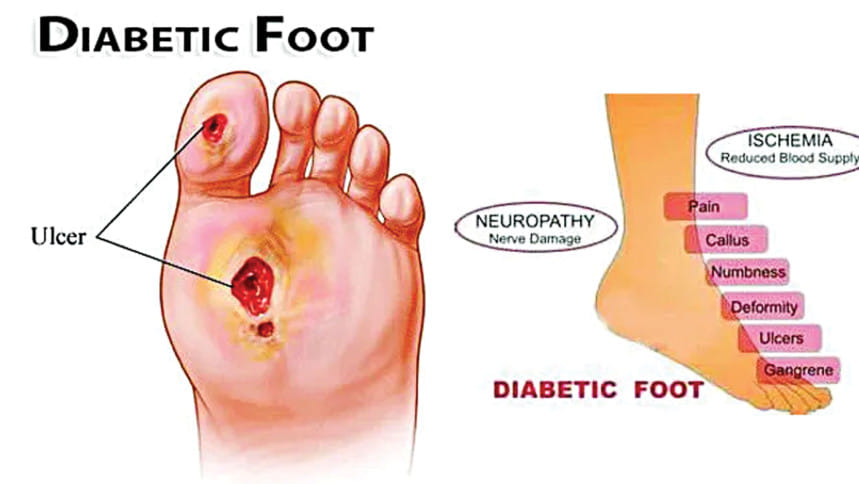
Diabetes-related foot infections (DFI) are increasingly common and can cause serious health issues. Recently, experts updated recommendations to help diagnose and manage these infections:
Severity and diagnosis: DFI severity depends on local and systemic symptoms. Doctors may sample tissue for culture using wound curettage or biopsy.
Diagnostic tools: X-rays and probe-to-bone tests might not always give a clear picture. In such cases, magnetic resonance imaging (MRI) is recommended.
Bone infections (Osteomyelitis): Culturing bone samples helps identify the bacteria causing bone infections. This can be done during surgery or through a minimally invasive procedure.
Antibiotic use: Antibiotics should not be used if there are no signs of infection in diabetic foot ulcers. Treatment for skin and soft tissue infections usually lasts 1-2 weeks, sometimes up to 4 weeks if improvement is slow.
Target bacteria: Initial treatment focuses on certain bacteria, especially Staphylococcus aureus. In some regions, coverage for Pseudomonas aeruginosa may be necessary.
Treatment duration: Patients with DFI-related bone infections might need antibiotics for 3 weeks after amputation or 6 weeks without amputation.
Surgical consideration: Surgery might be necessary for moderate to severe infections.
Adjunctive therapies: Some additional treatments, like growth factors, topical antiseptics, or hyperbaric oxygen, are not recommended.
Overall, these recommendations highlight the need for better access to quality healthcare for individuals dealing with DFI and ulcers.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments