Locally tailored policies and improved patient care systems are necessary next steps for Bangladesh during the pandemic
It was the last day of 2019, when the WHO's Country Office in China picked up a media statement—"a cluster of viral pneumonia was found in Wuhan, China". In the next nine months, that small cluster spread across the world to become a global pandemic, killing over a million and affecting billions of lives. The first case in Bangladesh was identified in early March, 2020. As of yesterday, there have been 370,132 cases identified and 5,375 recorded deaths. Each of these numbers carries a tale of tears—a tale of pain, frustration, agony and the loss of loved ones.
We have lost so many people primarily because there is no effective cure, treatment or a vaccine for this disease. While the medical and research communities are rushing to find one, so far the most effective strategy against Covid-19 is "social distancing" and "safe hygiene"—maintaining at least six feet distance from each other, using face masks, isolating the affected people and washing hands. The Bangladesh government emphasised on such practices and strictly implemented some from the very beginning. The initial response by the Bangladesh government was identified as one of the strict responses across the world based on indicators such as school closures, workplace closures and travel bans (according to the index created by scientific online publication Our World in Data, Bangladesh was placed at 80.09, with 100 being the strictest).
Most of the people in Bangladesh cooperated with the authorities and followed the guidelines in the early days. According to Our World in Data, the mobility trend in Bangladesh during the pandemic shows a significant drop in public movement. This ultimately slowed down disease transmission and provided the authorities with enough time to build healthcare infrastructure to fight the disease. The number of testing locations have been raised from one to 94, and there are now 30 hospitals for Covid-19 patients. Public policy and awareness, in addition to increased testing and treatment capacity, helped to reverse the trend of Covid-19 transmission even after lifting the lockdown in early June. A decrease in the percentage of positive cases was observed in August, according to a WHO update, while the number of daily tests remained consistent.
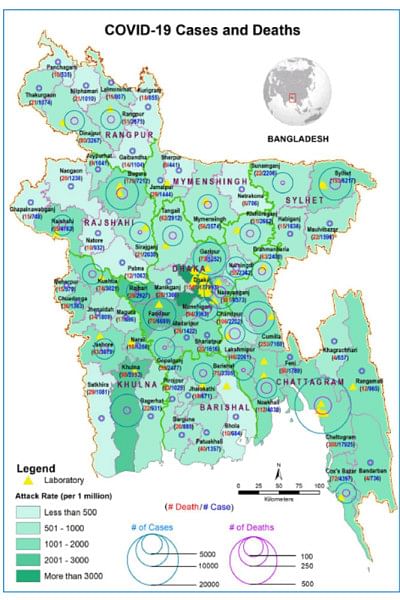
The overall downward trend in the daily Covid-19 cases is a good sign. However, in a country of 170 million people, it is critical to look at the trends at regional levels to identify any high-risk clusters in this massive population base. A locally tailored approach based on associated risks is necessary, especially during the reopening of the country, to prevent further outbreak and a possible second wave. In Bangladesh, one of the many regions that warrants such locally tailored policies is Mirpur, especially Pallabi in Dhaka city. Mirpur carries a significantly higher percentage of Covid-19 cases and Pallabi was found to follow a rapidly increasing trend while other areas in Mirpur observed some sorts of flattening curves. It is highly critical to identify such high-risk zones across the country and impose certain levels of local lockdowns while the other areas gradually reopen.
Besides the prevention strategy, it is also important to improve the patient care management system. Despite the downward trend in Covid-19 cases, the daily death toll remains consistent. In recent weeks, the number of weekly new cases decreased by 13.8 percent, however the weekly death toll increased by 10.8 percent. Chattogram was found to have the highest hospitalisation rate (27.4 percent) and highest relative death rate (21.6 percent death rate against 13.8 percent case rate) at the divisional level. A locally tailored healthcare approach based on stratified patients might also be helpful to identify the root causes behind such a high fatality rate and optimise the patient management system accordingly.
Patient care and public policies are currently the key strategies to fight this pandemic. These might help us survive during the waiting time to get to an effective vaccine. Typically, it takes more than a decade to develop a vaccine, however for Covid-19, the number of vaccines were moved to different stages of trials in less than a year. Extraordinary efforts have been put in place to collaborate among countries, academia, industry and health authorities to ensure vaccine availability whenever and wherever it is produced. The Bangladesh government has assured us on several occasions that its people will receive vaccines as soon as one becomes available at any corner in the world. The government is mainly relying on the vaccine allocation plan COVAX, which is led by GAVI, the WHO and CEPI to vaccinate around 20 percent of the world population once a vaccine is available. Prime Minister Sheikh Hasina, who was recognised as "Vaccine Hero" last year by GAVI, asked global leaders in the recent UN assembly to treat the vaccine as a "global public good" and stressed timely and equitable vaccine access. The government and local drug companies are also reaching out to potential vaccine manufacturers to get priority access to upcoming vaccines (if any) as well as to participate in clinical trials and research.
Vaccines have saved billions of lives throughout the history of mankind, not only protected the immunised people but also everyone else by preventing disease transmission. However, vaccines are just one of many strategies to fight infectious diseases like Covid-19. After 40 years of HIV infection, the world is yet to find any effective vaccine and HIV is far better managed and fatality rates are much lower today compared to earlier days. The primary strategies of self-containment, social distancing, lockdowns, patient care, hygiene and most importantly, public awareness, help tremendously to fight Covid-19. These approaches combined are found to reduce viral transmission and save lives. Some of these approaches, such as lockdowns, have been criticised for negative effects on the economy; however, saving lives or saving economies is a false dichotomy. No countries were able to minimise the impact on the economy at the expense of peoples' lives. In contrast, the economy followed the death tolls in a similar trend. The relative decreases in GDP were found to be highest in the countries that failed miserably to protect their people.
We have a long journey ahead with Covid-19 and "trust" is our safest and strongest boat to sail. No vaccine or policy is effective unless people have the trust to take it or follow it. In order to raise public trust in vaccine efforts, the leaders of the vaccine manufacturers have recently signed a safety pledge to follow strict safety protocols in the rush to vaccine development. The Bangladesh government has initiated various outreach efforts to educate, train and enlighten people and create public awareness. It's imperative to maintain and strengthen such efforts to ensure peoples' trust on the strategies and willingness to help each other in following healthcare guidelines. There is no alternative to working together as "No one is safe, unless everyone is safe" in this pandemic. It does not take much to wear a mask and ask others to do so to save their nearest and dearest ones.
As we move forward together, we will learn more about the disease, treatment, vaccine, policies and healthcare guidelines. The future will depend on how we can leverage these learnings to save peoples' lives.
Md Anik Alam is a Senior Scientist, R&D at Pfizer, US. The opinions in this article are those of the author and do not necessarily reflect the position of Pfizer. Email: anikalam_bd@yahoo.com

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments